Anti-cancer peptide, PNC-27, is a membrane-active peptide that binds to the HDM-2 protein expressed in the cancer cell membranes of solid tissue tumor cells. The peptide induces transmembrane pore formation in cancer, but not in normal cells, resulting in tumor cell necrosis (cell death).
PNC-27 has shown to be highly effective in selectively targeting a wide variety of specific forms of cancer, including pancreatic cancer, breast cancer, leukemia, melanoma, and additional cancer lines.
This is attributed to immunotherapy’s mechanism of utilizing the body’s own defense system, as opposed to absorbing harmful chemicals. Two forms of immunotherapy that have been effective in curing cancer without the added danger of chemical toxicity are PNC-27 and PNC-28. These peptides were created by a supercomputer at SUNY Downstate Medical Center in New York in 2000. PNC-27 and PNC-28 work with the MDM2 -P53 tumor suppressor complex. It acts as a competitive inhibitor for binding, increasing the half-life of P53 in the cell and assisting with the elimination of cancer cells (Sarafraz-Yazdi E, Bowne WB, et al 2010). These immunotherapy agents also have the ability to bind to the cell membrane and lyse the cell. The clinical trials for PNC-27 and 28 were successful. Research illustrates that this form of immunotherapy can be a successful strategy in eliminating the cancer and ensuring that a relapse does not occur.
Cancer cells have HDM-2 in their cell membranes. When the PNC-27 is administered, it immediately travels to the HDM-2 located in the membranes of cancerous cells. By binding to them, it creates pores or holes in the cell membrane causing death of the cell membrane. This, in turn, leads to the destruction of the cancer cell.
Research Example 1:
Methods: We have prepared PNC-27 with a green fluorescent label on its amino terminus and a red fluorescent label on its carboxyl terminus and treated MCF-7 breast cancer cells and untransformed MCF-10-2A breast epithelial cells with this double-labeled peptide to determine if combined yellow fluorescence occurs in the membrane of the cancer cells during cancer cell killing.
Results: At 30 min, there is significant combined punctate yellow fluorescence, indicative of intact peptide, in the cell membrane of cancer cells that increases during cancer cell lysis. MCF-10-2A cells show initial (30 min) uniform combined yellow membrane fluorescence that subsequently disappears. Unlike the cancer cells, these untransformed cells remain viable.
Conclusions: PNC-27 induces cancer cell membrane lysis by acting as the whole peptide, not fragments. The punctate yellow fluorescence is due to interaction of PNC-27 with intramembrane targets of MCF-7 cells that do not exist in the membrane of the untransformed cell line. This interaction increases the lifetime of PNC-27. Absence of these targets in the membranes of the untransformed MCF-10-2A cells results in initial uniform fluorescence of the double-labeled peptide in their membranes, after which the peptide is degraded.
Research Example 2:
Research Example 3:
Methods: SKOV3-luc-D3 cells were cultured, passed and maintained in our lab. MTT & LDH assays were performed to assess cytotoxicity of PNC-27 versus a control peptide. For the MTD, daily bolus IP injections of PNC-27 were injected into healthy female nu/nu mice. Toxicities were assessed by body condition score (BCS) and sluggishness scale (SS). A 3 + 3 up-and-down design was used to determine the MTD of PNC-27. Finally, SKOV3-luc-D3 cells were injected IP into female nu/nu mice. Tumor burden was assessed via BCS and weight change. Once adequate tumor load was established, the mice were treated with PNC-27 at either the MTD (n = 5) or one level below the MTD (n = 5). The toxicity of PNC-27 was examined by BCS, SS and histopathologic sectioning.
Results: PNC-27 successfully suppressed cell proliferation (measured by MTT assay) and was cytotoxic (measured by LDH assay) as compared to a control peptide in vitro. The MTD of IP bolus injections of PNC-27 was 2 mg/day. Dose limiting toxicities (DLT) were met in 2/3 mice at
4 mg/day and 2/6 mice in the expanded cohort at 3 mg/day. Complete resolution of DLTs took 7 days. Finally, tumor burden after IP injection was determined via palpable and visible abdominal tumors present on the mice, as there were no significant differences in weight or BCS. The mice with clinically apparent tumor tolerated treatment at both the 1.5 mg/day and 2 mg/day levels. Histopathologic assessment confirmed these findings.
Conclusions: PNC-27 has cytostatic and cytotoxic effects on the SKOV3-luc-D3 cell line in vitro. The MTD of PNC-27 in the nu/nu mice via bolus intraperitoneal daily injection is 2 mg/day in both healthy mice and those with tumor burden. Future research with the SKOV3-luc-D3 cell line will utilize the bioluminescent component of the cells to follow tumor development and clinical response to the maximum tolerated dose of PNC-27 without the need to kill the animal to obtain such measurements.
Research Example 4:
Methods: We established primary cultures of freshly isolated epithelial ovarian cancer cells from patients with newly diagnosed ovarian cystadenocarcinomas. Two cell lines were obtained, one from mucinous cystadenocarcinoma, and the other from high-grade papillary serous carcinoma. The cancerous properties of these cells were characterized in vitro morphologically, by their growth requirements and serum independence. Treatment effects with PNC-27 were followed qualitatively by light microscopy, and quantitatively by measuring inhibition of cell growth using the MTT cell proliferation assay and direct cytotoxicity by measuring lactate dehydrogenase (LDH).
Results: PNC-27 inhibits in a dose-dependent manner the growth of and is cytotoxic to human primary cancer cells that had been freshly isolated from two ovarian epithelial cancers. The results further show that the control peptide PNC-29 has no effect on the primary cancer cells. Our results also show that PNC-27 is cytotoxic to cells from long-established and chemotherapy-resistant human ovarian cancer cell lines.
Conclusion: These findings show, for the first time, the efficacy of PNC-27 on freshly isolated, primary human cancer cells. Our results indicate the potential of PNC-27 peptide as an efficient alternative treatment of previously untreated ovarian cancer as well as for ovarian cancers that have become resistant to present chemotherapies.
PNC-27 has shown to be highly effective in selectively targeting a wide variety of specific forms of cancer, including pancreatic cancer, breast cancer, leukemia, melanoma, and additional cancer lines.
What is PNC-27?
Immunotherapeutic agents have been researched for many decades as an alternative treatment for cancer. Current research demonstrates that immunotherapy is safer than radiotherapy or chemotherapy.This is attributed to immunotherapy’s mechanism of utilizing the body’s own defense system, as opposed to absorbing harmful chemicals. Two forms of immunotherapy that have been effective in curing cancer without the added danger of chemical toxicity are PNC-27 and PNC-28. These peptides were created by a supercomputer at SUNY Downstate Medical Center in New York in 2000. PNC-27 and PNC-28 work with the MDM2 -P53 tumor suppressor complex. It acts as a competitive inhibitor for binding, increasing the half-life of P53 in the cell and assisting with the elimination of cancer cells (Sarafraz-Yazdi E, Bowne WB, et al 2010). These immunotherapy agents also have the ability to bind to the cell membrane and lyse the cell. The clinical trials for PNC-27 and 28 were successful. Research illustrates that this form of immunotherapy can be a successful strategy in eliminating the cancer and ensuring that a relapse does not occur.
How does PNC-27 work?
Cancer cells have HDM-2 in their cell membranes. When the PNC-27 is administered, it immediately travels to the HDM-2 located in the membranes of cancerous cells. By binding to them, it creates pores or holes in the cell membrane causing death of the cell membrane. This, in turn, leads to the destruction of the cancer cell.
Research Example 1:
The anti-cancer peptide, PNC-27, induces tumor cell lysis as the intact peptide
Purpose: PNC-27, a peptide that contains an HDM-2-binding domain from p53 attached to a membrane-penetrating peptide on its carboxyl terminal end, is cytotoxic to cancer, but not normal, cells. It forms transmembrane pores in the cancer cell membrane. Our purpose is to determine if the whole peptide or critical fragments induce pore formation in cancer cells.Methods: We have prepared PNC-27 with a green fluorescent label on its amino terminus and a red fluorescent label on its carboxyl terminus and treated MCF-7 breast cancer cells and untransformed MCF-10-2A breast epithelial cells with this double-labeled peptide to determine if combined yellow fluorescence occurs in the membrane of the cancer cells during cancer cell killing.
Results: At 30 min, there is significant combined punctate yellow fluorescence, indicative of intact peptide, in the cell membrane of cancer cells that increases during cancer cell lysis. MCF-10-2A cells show initial (30 min) uniform combined yellow membrane fluorescence that subsequently disappears. Unlike the cancer cells, these untransformed cells remain viable.
Conclusions: PNC-27 induces cancer cell membrane lysis by acting as the whole peptide, not fragments. The punctate yellow fluorescence is due to interaction of PNC-27 with intramembrane targets of MCF-7 cells that do not exist in the membrane of the untransformed cell line. This interaction increases the lifetime of PNC-27. Absence of these targets in the membranes of the untransformed MCF-10-2A cells results in initial uniform fluorescence of the double-labeled peptide in their membranes, after which the peptide is degraded.
Research Example 2:
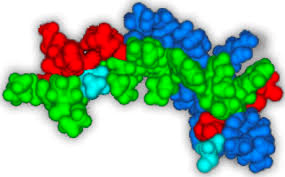
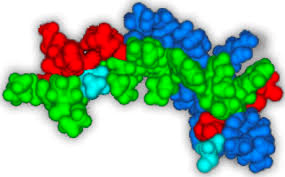
Anticancer peptide PNC-27 adopts an HDM-2-binding conformation and kills cancer cells by binding to HDM-2 in their membrane
The anticancer peptide PNC-27, which contains an HDM-2-binding domain corresponding to residues 12-26 of p53 and a transmembrane-penetrating domain, has been found to kill cancer cells (but not normal cells) by inducing membranolysis. We find that our previously determined 3D structure of the p53 residues of PNC-27 is directly superimposable on the structure for the same residues bound to HDM-2, suggesting that the peptide may target HDM-2 in the membranes of cancer cells. We now find significant levels of HDM-2 in the membranes of a variety of cancer cells but not in the membranes of several untransformed cell lines. In colocalization experiments, we find that PNC-27 binds to cell membrane-bound HDM-2. We further transfected a plasmid expressing full-length HDM-2 with a membrane-localization signal into untransformed MCF-10-2A cells not susceptible to PNC-27 and found that these cells expressing full-length HDM-2 on their cell surface became susceptible to PNC-27. We conclude that PNC-27 targets HDM-2 in the membranes of cancer cells, allowing it to induce membrane lysis of these cells selectively.Research Example 3:
Evaluation of PNC-27-mediated toxicity in an intraperitoneal mouse model of human ovarian cancer
Objectives: PNC-27 is a novel anti-cancer peptide explicitly cytotoxic against cancer cells via formation of trans-membrane pores while sparing normal cells. We sought to determine the effect of PNC-27 on the established ovarian cancer cell line SKOV3-luc-D3 in vitro. Then, utilizing murine nu/nu mouse models, we sought to determine the maximum tolerated dose (MTD) of daily bolus intraperitoneal (IP) injections in healthy mice and finally to determine the toxicity of PNC- 27 around the determined MTD using SKOV3-luc-D3 cells in vivo.Methods: SKOV3-luc-D3 cells were cultured, passed and maintained in our lab. MTT & LDH assays were performed to assess cytotoxicity of PNC-27 versus a control peptide. For the MTD, daily bolus IP injections of PNC-27 were injected into healthy female nu/nu mice. Toxicities were assessed by body condition score (BCS) and sluggishness scale (SS). A 3 + 3 up-and-down design was used to determine the MTD of PNC-27. Finally, SKOV3-luc-D3 cells were injected IP into female nu/nu mice. Tumor burden was assessed via BCS and weight change. Once adequate tumor load was established, the mice were treated with PNC-27 at either the MTD (n = 5) or one level below the MTD (n = 5). The toxicity of PNC-27 was examined by BCS, SS and histopathologic sectioning.
Results: PNC-27 successfully suppressed cell proliferation (measured by MTT assay) and was cytotoxic (measured by LDH assay) as compared to a control peptide in vitro. The MTD of IP bolus injections of PNC-27 was 2 mg/day. Dose limiting toxicities (DLT) were met in 2/3 mice at
4 mg/day and 2/6 mice in the expanded cohort at 3 mg/day. Complete resolution of DLTs took 7 days. Finally, tumor burden after IP injection was determined via palpable and visible abdominal tumors present on the mice, as there were no significant differences in weight or BCS. The mice with clinically apparent tumor tolerated treatment at both the 1.5 mg/day and 2 mg/day levels. Histopathologic assessment confirmed these findings.
Conclusions: PNC-27 has cytostatic and cytotoxic effects on the SKOV3-luc-D3 cell line in vitro. The MTD of PNC-27 in the nu/nu mice via bolus intraperitoneal daily injection is 2 mg/day in both healthy mice and those with tumor burden. Future research with the SKOV3-luc-D3 cell line will utilize the bioluminescent component of the cells to follow tumor development and clinical response to the maximum tolerated dose of PNC-27 without the need to kill the animal to obtain such measurements.
Research Example 4:
Ex vivo Efficacy of Anti-Cancer Drug PNC-27 in the Treatment of Patient-Derived Epithelial Ovarian Cancer
Objective: Despite an 80% response rate to chemotherapy, epithelial ovarian cancer has the highest case fatality rate of all gynecologic malignancies. Several studies have shown the efficiency of anticancer peptides PNC-27 and PNC-28 in killing a variety of cancer cells selectively in vitro and in vivo. The purpose of this study was to evaluate the efficacy of PNC-27 against human primary epithelial ovarian cancer.Methods: We established primary cultures of freshly isolated epithelial ovarian cancer cells from patients with newly diagnosed ovarian cystadenocarcinomas. Two cell lines were obtained, one from mucinous cystadenocarcinoma, and the other from high-grade papillary serous carcinoma. The cancerous properties of these cells were characterized in vitro morphologically, by their growth requirements and serum independence. Treatment effects with PNC-27 were followed qualitatively by light microscopy, and quantitatively by measuring inhibition of cell growth using the MTT cell proliferation assay and direct cytotoxicity by measuring lactate dehydrogenase (LDH).
Results: PNC-27 inhibits in a dose-dependent manner the growth of and is cytotoxic to human primary cancer cells that had been freshly isolated from two ovarian epithelial cancers. The results further show that the control peptide PNC-29 has no effect on the primary cancer cells. Our results also show that PNC-27 is cytotoxic to cells from long-established and chemotherapy-resistant human ovarian cancer cell lines.
Conclusion: These findings show, for the first time, the efficacy of PNC-27 on freshly isolated, primary human cancer cells. Our results indicate the potential of PNC-27 peptide as an efficient alternative treatment of previously untreated ovarian cancer as well as for ovarian cancers that have become resistant to present chemotherapies.
